Aspergillosis
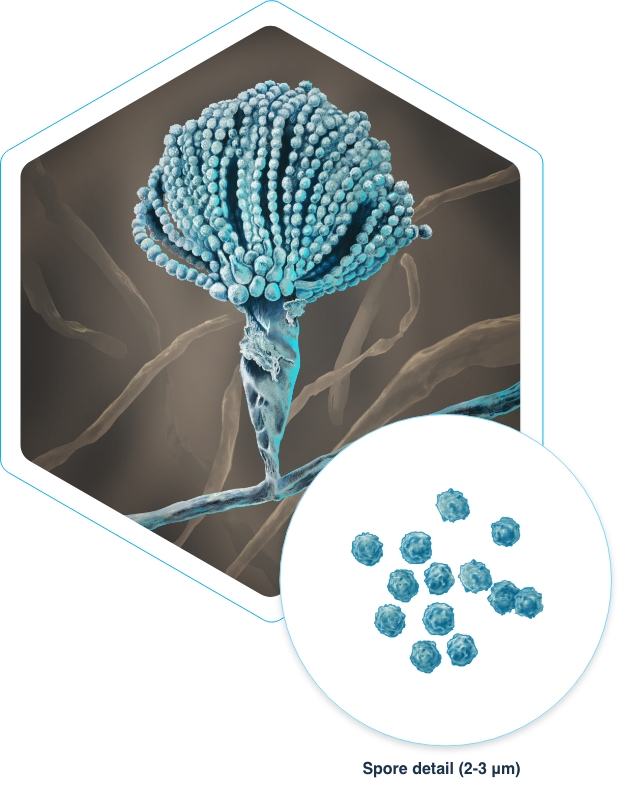
What is Aspergillus?
Aspergillus is a genus of fungi that has evolved to grow and survive under many environmental conditions worldwide. While it is often found outside in soil and on plants, trees, and compost, Aspergillus can also be found indoors in air conditioning systems and carried on people and pets.
There are more than 180 species of Aspergillus but fewer than 40 have been found to cause disease in humans.1 Most infections resulting from the fungus are caused by the Aspergillus fumigatus species.1
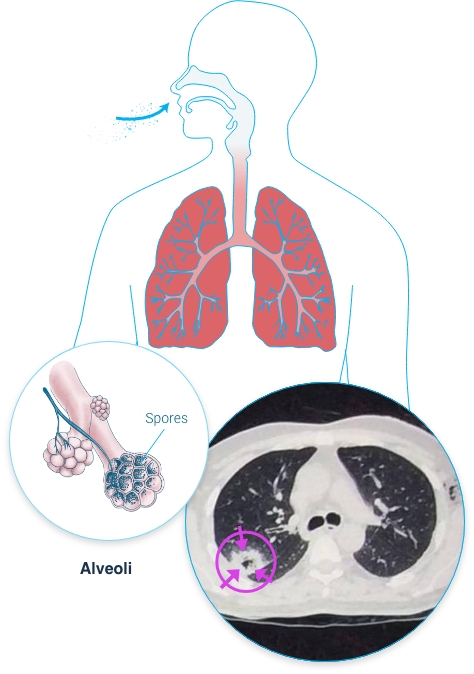
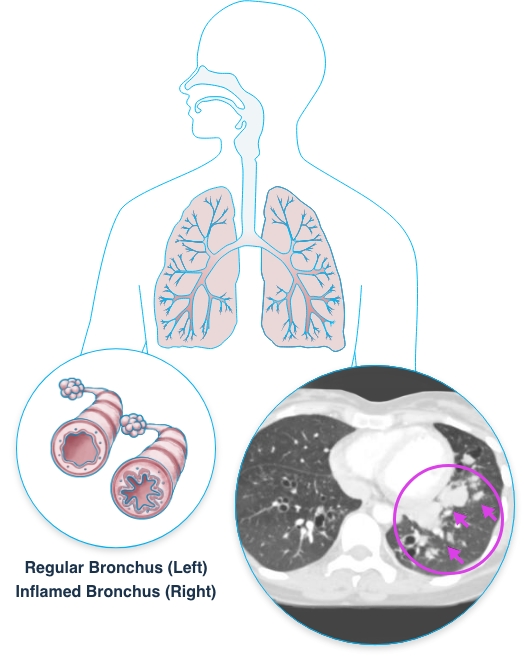
Aspergillus fungi are easily spread through the air. Aspergillus spores are small and typically measure 2 µm to 3 µm in size.2 This means that when these fungal spores are inhaled by a person, they are small enough to potentially reach all parts of the respiratory system, from the upper airways down to the distal portion of the lower airways in the lungs.2 In people with weakened immune systems or with pre-existing lung disease, the Aspergillus spores in the airways and lung tissue can lead to severe lung disease that is often life threatening.
Aspergillus can cause a range of diseases collectively called “aspergillosis.” Because Aspergillus is often introduced into the body via the airways, pulmonary aspergillosis (aspergillosis in the lungs) is the most common form of the disease. However, less commonly, aspergillosis may start in locations other than the lungs, such as the sinuses, gastrointestinal tract, or skin (via intravenous catheters or prolonged skin contact with adhesive tapes or burns).3 While rare, when the disease invades the blood vessels, Aspergillus infection may spread to other organs such as the brain, heart, and kidneys. This is known as disseminated aspergillosis.3
What is Pulmonary Aspergillosis?
Pulmonary aspergillosis can present as different disease types, depending on the patient’s underlying health status. For example, in patients with pre-existing cavitary lung disease, Aspergillus infection can cause an aspergilloma, or a fungal ball, to grow in one or several of these cavities. In patients with chronic lung diseases such as chronic obstructive pulmonary disease (COPD) or those who are mildly immunocompromised, Aspergillus infection can cause chronic necrotizing aspergillosis. In those who are more severely immunocompromised, pulmonary aspergillosis can be invasive, known as invasive pulmonary aspergillosis. This is the most severe and life-threatening form of aspergillosis and tends to affect patients with an underlying hematological malignancy, recipients of a stem cell transplant, or recipients of a solid organ transplant, most notably lung transplant recipients. Finally, in patients with asthma or with cystic fibrosis, the presence of Aspergillus in the patient’s airways can cause a severe hypersensitive or allergic reaction leading to a form of aspergillosis called severe asthma with fungal sensitization or allergic bronchopulmonary aspergillosis.
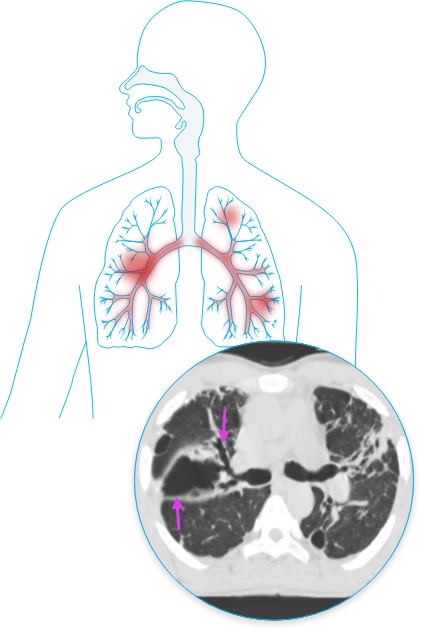
Invasive Pulmonary Aspergillosis (IPA)
IPA is the most severe form of pulmonary aspergillosis. It is a serious and life-threatening Aspergillus infection of the lungs, marked by fungal lung tissue invasion and destruction that can spread to other parts of the body. IPA typically affects people who are severely immunocompromised or have weakened immune systems, such as patients with an underlying hematological malignancy, recipients of a stem cell transplant, or recipients of a solid organ transplant, most notably lung transplant recipients. Other patients who may also be susceptible to IPA include immunocompetent patients who do not have the classic risk factors for invasive disease, such as patients with severe COPD and critically ill patients in the intensive care unit (ICU).3 During and following the recent SARS-CoV-2 pandemic, reports of COVID-19-associated pulmonary aspergillosis raised concerns about it worsening the disease course of COVID-19 and increasing mortality, particularly for patients in the ICU.4
The growing use of chemotherapy and immunosuppressants, along with the rise in stem cell and solid organ transplants, have contributed to the rising incidence of IPA.3 Even with the availability of approved standard-of-care antifungal treatment, the mortality rate in patients with invasive aspergillosis remains high, and the overall mortality rate at one year is approximately 50% and can reach 90% in patients who have received a hematopoietic stem cell transplant despite use of first-line antifungal therapy.3,5
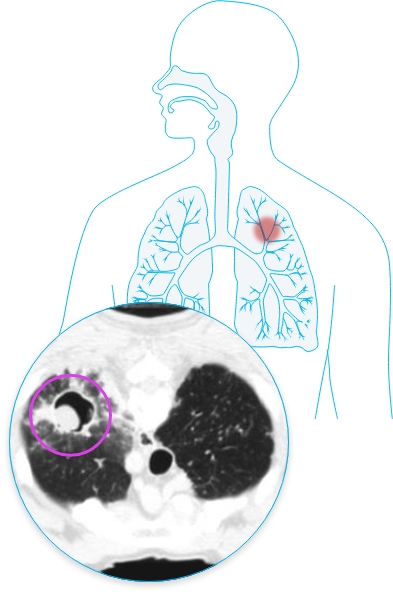
Image source: Invasive pulmonary aspergillosis on a CT scan of the chest in a 35-year-old male with confirmed Aspergillus fumigatus infection. The CT scan shows breakdown within a consolidation of the lower lobe in the right lung.*
Aspergilloma
An aspergilloma, or fungus ball, is typically a noninvasive disease that occurs when Aspergillus colonizes a preexisting pulmonary cavity or a dilated bronchus. This form of disease may occur in patients with abnormal airways (COPD, bronchiectasis, cystic fibrosis) or in those with chronic lung cavities, such as patients with tuberculosis, sarcoid-related pulmonary cavities, or emphysema.
Chronic Necrotizing Pulmonary Aspergillosis (CPA or CNA)
CPA is an invasive Aspergillus infection of the lungs similar to IPA, but CPA is a slow-progressing disease that does not typically spread to other organs. CPA is typically found in patients with chronic lung disease such as COPD, previous pulmonary tuberculosis, sarcoidosis, previous lung surgery, and pneumoconiosis.6 It may also occur in patients with mild immunodeficiency such as those receiving long-standing steroid therapy or in patients with diabetes or renal failure.7 As with other forms of pulmonary aspergillosis, CPA can be difficult to properly treat and patients with CPA may relapse, needing prolonged or lifelong treatment.8
Allergic Bronchopulmonary Aspergillosis (ABPA) and Severe Asthma With Fungal Sensitization (SAFS)
ABPA is a noninvasive form of pulmonary aspergillosis. Unlike IPA, which is marked by fungal lung tissue invasion and destruction, ABPA is characterized by a hypersensitive allergic inflammatory response to Aspergillus in the lungs. It is typically found in patients with asthma or cystic fibrosis.3 This response can cause lasting damage to the patient’s lungs with pathological dilation of the airways and scarring, further impairing lung function and quality of life.3 In patients with asthma, uncontrolled ABPA can lead to frequent asthma exacerbations that may require hospitalization.
SAFS is similar to ABPA, in that it describes people with persistent severe asthma and evidence of fungal sensitization. However, patients with SAFS tend to have a less severe allergic response and do not meet all the diagnostic criteria for ABPA.
How is Aspergillosis Diagnosed?
Depending on the patient’s characteristics and type of Aspergillus disease, the diagnostic tests for aspergillosis can include:
Imaging of the respiratory system with a CT scan
Testing of the blood or a sample of airway fluid taken during a bronchoscopy for biomarkers, including galactomannan
Fungal staining and evaluation under a microscope of tissue samples for the presence of fungal elements
Fungal culture of a sputum sample, a tissue sample taken from a biopsy, or a fluid sample taken from the patient’s airways during a bronchoscopy
Tissue nucleic acid diagnosis for Aspergillus by PCR combined with DNA sequencing on a blood or tissue sample or a sample of airway fluid taken during bronchoscopy
How is Aspergillosis Treated?
Approved treatments for pulmonary aspergillosis consist of three main classes of antifungal agents that are administered to the patient either orally or intravenously: triazoles, echinocandins, and polyenes.
First-line antifungal treatment for aspergillosis typically includes a medication from the triazole class. The choice of antifungal medication is based on many factors, including the patient’s state of health and the potential side effects of antifungal medications. Current clinical guidelines recommend initial therapy with voriconazole, either on its own or in combination with another antifungal.9
Even with current treatments, the prognosis for patients with invasive aspergillosis can be poor. For example, in a Phase 3 trial evaluating the safety and efficacy of isavuconazole, the most recently approved triazole, versus voriconazole as a treatment for patients with proven or probable invasive aspergillosis, both groups saw less than 40% of patients assessed as having overall success at the end of treatment.10 This clinical trial observation suggests that the majority of patients with invasive aspergillosis may require some form of second line treatment, as they could have refractory disease, which could include changing or adding to the antifungal regimen or reducing the level of immunosuppression.
Some classes of antifungals used to treat aspergillosis have been associated with a number of serious toxicities and drug-drug interactions. These may limit their utility in treating aspergillosis and can also compromise treatment options for oncology and transplant patients.11